PUBLICATIONS
Dr. Madácsy László - publicatons
Authors: Dr. Madácsy László
Dr. Madácsy László - idézhető előadás kivonatok és folyóirat közlemények.
Published contributions to academic conferences (abstracts): 163
In extenso Pubications (folyóirat közlemények): 43
Összesített impact faktor: 69,323
full article »»»

Association between visceral, cardiac and sensorimotor polyneuropathies in diabetes mellitus.
Authors: Søfteland E, Brock C, Frøkjær JB, Brøgger J, Madácsy L, Gilja OH, Arendt-Nielsen L, Simrén M, Drewes AM, Dimcevski G.
J Diabetes Complications. 2013 Oct 29. pii: S1056-8727(13)00275-4. doi: 10.1016
ABSTRACT: AIMS: Gastrointestinal complaints are common in diabetes mellitus. However, its association to peripheral sensorimotor and autonomic neuropathies is not well investigated. The aim was to assess skin, muscle, bone and visceral sensitivity in diabetes patients with sensorimotor neuropathy, and correlate these with gastrointestinal symptoms and degree of cardiac autonomic neuropathy.
METHODS: Twenty patients with sensorimotor neuropathy (65% type 2 diabetes, aged 58.3±12.0years, diabetes duration 15.8±10.0years) and 16 healthy controls were recruited. Cutaneous sensitivity to von Frey filaments, mechanical allodynia, muscle/bone/rectosigmoid sensitivities, and heart rate variability were examined. Gastrointestinal symptom scores (PAGI-SYM) and health-related quality of life (SF-36) were also recorded.
RESULTS: Patients displayed hypesthesia to von Frey filaments (p=0.028), but no difference to muscle and bone pain sensitivities. Also, patients were hyposensitive to multimodal rectal stimulations (all p<0.05), although they suffered more gastrointestinal complaints. Heart rate variability was reduced in the patient cohort. Rectal mechanical and cutaneous sensitivities correlated (p<0.001), and both were associated with heart rate variability as well as PAGI-SYM and SF-36 scores (p<0.01).
CONCLUSIONS: In diabetic sensorimotor neuropathy there is substantial evidence of concomitant cutaneous, cardiac and visceral autonomic neuropathies. The neuropathy may reduce quality of life and explain the higher prevalence of gastrointestinal complaints.
full article »»»
Endoscopic transluminal pancreatic necrosectomy using a self-expanding metal stent and high-flow water-jet system
Authors: István Hritz, Roland Fejes, András Székely, Iván Székely, László Horváth, Ágnes Sárkány, Áron Altorjay, László Madácsy
Walled-off pancreatic necrosis and a pancreatic abscess
are the most severe complications of acute pancreatitis.
Surgery in such critically ill patients is often associated
with significant morbidity and mortality within the first
few weeks after the onset of symptoms. Minimal invasive
approaches with high success and low mortality
rates are therefore of considerable interest. Endoscopic
therapy has the potential to offer safe and effective
alternative treatment. We report here on 3 consecutive
patients with infected walled-off pancreatic necrosis
and 1 patient with a pancreatic abscess who underwent
direct endoscopic necrosectomy 19-21 d after the onset
of acute pancreatitis. The infected pancreatic necrosis
or abscess was punctured transluminally with a cystostome
and, after balloon dilatation, a non-covered self-expanding biliary metal stent was placed into the
necrotic cavity. Following stent deployment, a nasobiliary
pigtail catheter was placed into the cavity to ensure
continuous irrigation. After 5-7 d, the metal stent was
removed endoscopically and the necrotic cavity was
entered with a therapeutic gastroscope. Endoscopic
debridement was performed via the simultaneous application
of a high-flow water-jet system; using a flush
knife, a Dormia basket, and hot biopsy forceps. The
transluminal endotherapy was repeated 2-5 times daily
during the next 10 d. Supportive care included parenteral
antibiotics and jejunal feeding. All patients improved
dramatically and with resolution of their septic
conditions; 3 patients were completely cured without
any further complications or the need for surgery. One
patient died from a complication of prolonged ventilation
severe bilateral pneumonia, not related to the endoscopic
procedure. No procedure related complications
were observed. Transluminal endoscopic necrosectomy
with temporary application of a self-expanding metal
stent and a high-flow water-jet system shows promise
for enhancing the potential of this endoscopic approach
in patients with walled-off pancreatic necrosis and/or a
pancreatic abscess.
full article »»»

Assessment of the reproducibility of quantitative hepatobiliary scintigraphy (QHBS) in patients with sphincter of Oddi dysfunction (SOD)--inappropriate method or intermittent disease?
Authors: Bertalan V, Szepes A, Lonovics J, Madácsy L.
Abstract
BACKGROUND/AIMS: Although quantitative hepatobiliary scintigraphy (QHBS) was originally suggested as a promising method in the diagnosis of sphincter of Oddi dysfunction (SOD), it was recently claimed that QHBS displays poor reproducibility and specificity in cholecystectomized patients. The aim of the present study was to assess the reproducibility of QHBS in cholecystectomized patients.
METHODOLOGY: 28 cholecystectomized patients with suspected SOD underwent QHBS evaluation on two separate occasions. On the basis of the clinical and endoscopic retrograde cholangiopancreatography (ERCP) data, patients with suspected SOD were categorized by applying the Geenen and Hogan classification: 10 were identified as having SOD of biliary type I (SO stenosis group), and the remaining 18 patients as having SOD of biliary type II or III (SO dyskinesia group). During the same period, 12 asymptomatic cholecystectomized individuals (control group) were recruited to undergo QHBS evaluation on two separate occasions. QHBS was performed with our standard method in all subjects. After an overnight fast, 140MBq 99mTc-EHIDA was injected intravenously. Digital images were recorded continuously on a 128 x 128 matrix, at one frame/min for 90 min. For the final analysis, the liver-choledochus T. difference (LCTD), half-time of excretion of the common bile duct (CBD T1/2), and the duodenum appearance time (DAT) were applied.
RESULTS: In the 12 asymptomatic controls, the QHBS parameters were highly reproducible, all but 6 of the 72 separate parameters obtained from two repeated studies were within our normal limits. In all 10 patients belonging in the SO stenosis group, the QHBS parameters were markedly abnormal and again highly reproducible. All of the 60 separate quantitative parameters obtained in this group from the two repeated studies were high above our normal range. In contrast, in the 18 patients with SO dyskinesia, the QHBS parameters were distinctly variable and poorly reproducible. Of the 108 separate quantitative parameters obtained in this group the two separate studies, 55 were normal and 53 were above our normal range. Of the 18 SO dyskinesia patients, only 9 had at least one quantitative parameter abnormal in both QHBS examinations.
CONCLUSIONS: QHBS is a highly reproducible technique in cholecystectomized controls and in patients with SO stenosis. In contrast, the reproducibility of QHBS is poor in patients with SO dyskinesia, which is probably a consequence of the disease characteristics rather than methodological insufficiency of QHBS.
full article »»»
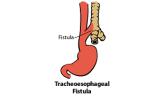
Recurrent, nonmalignant tracheoesophageal fistulas and the need for surgical improvisation.
Authors: Altorjay A, Mucs M, Rüll M, Tihanyi Z, Hamvas B, Madácsy L, Paál B.
Abstract
BACKGROUND: Despite the many recent advances in thoracic surgery, the management of patients with recurrent, nonmalignant tracheoesophageal fistulas remains problematic, controversial, and challenging.
METHODS: Between 1998 and 2008, we treated 8 patients with RTEF. Closure of the original tracheoesophageal fistula had been attempted once in 5 patients, twice in 2 patients, and 4 times in 1 patient, all in different institutions. Four cases necessitated right posterolateral thoracotomy and cervical exposure, 2 cases cervical and abdominal incision, and 1 case right posterolateral thoracotomy, with abdominal and cervical exposure. With the exception of the 2 patients whose excluded esophagus was used to substitute for the trachea membranous wall, the damaged tracheal segment was removed. In general, a pedicled mediastinal pleural flap was pulled into the neck to increase the safety of the tracheal anastomosis formed with the trachea, and (or) to separate the suture lines of the two organs.
RESULTS: A single intervention was sufficient for all 8 patients: no reoperation was necessary, and there was no perioperative mortality. Transient reflux, abdominal distention, and dyspnea in response to forced physical exertion occurred in 1 case each. Only 1 patient subsequently takes medication regularly for reflux disease.
CONCLUSIONS: Separation initiated from the tracheal bifurcation, a pedicled mediastinal pleural flap pulled into the neck, a tracheal anastomosis sewn onto the cricoid cartilage with avoidance of its posterolateral elbow, a shaped Dumon stent (Novatech, Plan de Grasse, France) with an individually fenestrated tracheostomy cannula, and endoscopy-assisted, transhiatal vagal-preserving esophageal exclusion all served as successful elements of our surgical procedures.
2010 The Society of Thoracic Surgeons. Published by Elsevier Inc. All rights reserved.
full article »»»

Early ERCP and biliary sphincterotomy with or without small-caliber pancreatic stent insertion in patients with acute biliary pancreatitis: better overall outcome with adequate pancreatic drainage.
Authors: Dubravcsik Z, Hritz I, Fejes R, Balogh G, Virányi Z, Hausinger P, Székely A, Szepes A, Madácsy L.
Abstract
OBJECTIVE: To analyze the efficacy of pancreatic duct (PD) stenting following endoscopic sphincterotomy (EST) compared with EST alone in reducing complication rate and improving overall outcome in acute biliary pancreatitis (ABP).
METHODS: Between 1 January 2009 and 1 July 2010, 141 nonalcoholic patients with clinical, laboratory and imaging evidence of ABP were enrolled. Emergency endoscopic retrograde cholangiopancreatography (ERCP) was performed within 72 h from the onset of pain. Seventy patients underwent successful ERCP, EST, and stone extraction (control group); 71 patients (PD stent group) had EST, stone extraction and small-caliber (5 Fr, 3-5 cm) pancreatic stent insertion. All patients were hospitalized for medical therapy and jejunal feeding and were followed up.
RESULTS: The mean age, Glasgow score, symptom to ERCP time, mean amylase and CRP levels at initial presentation were not significantly different in the PD stent group compared to the control group: 60.6 vs. 64.3, 3.21 vs. 3.27, 34.4 vs. 40.2, 2446.9 vs. 2114.3, 121.1 vs. 152.4, respectively. Complications (admission to intensive care unit, pancreatic necrosis with septicemia, large (>6 cm) pseudocyst formation, need for surgical necrosectomy) were less frequent in the PD stent group resulting in a significantly lower overall complication rate (9.86% vs. 31.43%, p < 0.002). Mortality rates (0% vs. 4.28%) were comparable, reasonably low and without any significant differences.
CONCLUSIONS: Temporary small-caliber PD stent placement may offer sufficient drainage to reverse the process of ABP. Combined with EST the process results in a significantly less complication rate and better clinical outcome compared with EST alone during the early course of ABP.
full article »»»

Does removal of prophylactic pancreatic stents induce acute pancreatitis?
Authors: Hritz I, Dubravcsik Z, Szepes A, Madácsy L.
Comment on Acute pancreatitis after removal of retained prophylactic pancreatic stents. [Gastrointest Endosc. 2011]
full article »»»

Endoscopic submucosal dissection performed in livE pig models and in humans with large, laterally spreading gastric and colorectal adenomas - Assessment of the initial learning curves, success rate and complications
Authors: Balogh G Jr, Dubravcsik Z, Szepes A, Madácsy L
Endoscopic submucosal dissection is a promising new endoscopic technique for en block resection of early, superficial, flat, and laterally spreading gastrointestinal neoplasms. The primary aims of this prospective study were to summarize the first Hungarian experience with endoscopic submucosal dissection, and to compare the experimental in vivo procedures in pigs with the human application of this technique in two academic centers. Methods: The ex vivo Erlangen pig model was used until initial competence was achieved. Thereafter 15 endoscopic submucosal dissection procedures were performed in up to 5 sessions in living pigs under general anesthesia. After submucosal injection with saline Fujinone ball tip, a Flush knife was used with a transparent hood for circumferential incision and submucosal dissection. The following variables were analyzed: specimen size, complete and en bloc resection rate, total duration of the procedure, and complications. Furthermore, between 2009 and 2012, 14 endoscopic submucosal dissections were carried out in humans; 1 duodenal, 3 gastric and 10 colorectal interventions were performed due to large laterally spreading intramucosal neoplasms. The specimen size, en bloc resection rate, total duration of the procedure and complications were next analyzed. Results: 87% complete resection rate, 29.4±19.5 cm2 specimen size and 136.2±26.8 min of procedure duration were achieved in the live pig models. Nontransmural damages of the muscular layer occurred in 3/15 (20%) cases which were successfully closed with hemoclips, except in one pig that died due to fatal esophageal perforation. All bleedings were easily managed with hot biopsy forceps coagulation and hemoclips without hemodynamic instability. In humans, endoscopic submucosal dissection was accomplished with an 11/14 (79%) en block resection rate, with average resected specimen size of 11.56±4.9 cm2 and with 157±55 min of operating time. Two cases of bleeding and 2 cases of perforation occurred (14%), all of which were managed endoscopically. After 1.5 year of average follow up, local recurrence occurred in one case only. In addition, due to the 3 incomplete resections and unsuccessful endoscopic submucosal dissection, surgical intervention was required in 4 cases altogether. Conclusions: This study demonstrates the first Hungarian experience with endoscopic submucosal dissection. Training in live pig models could help endoscopists to overcome the learning curve and minimize the risk of complications before starting the procedure in humans. Reduction in the resection time and low risk of complications, especially bleeding, could be achieved by the application of a flush knife
full article »»»
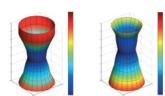
A new distensibility technique to measure sphincter of Oddi function
Authors: P. KUNWALD, A. M. DREWES, D. KJÆR, F. H. GRAVESEN, B. P. MCMAHON, L. MADÁCSY, P. FUNCH-JENSEN, H. GREGERSEN
Background Evaluation of the biliary tract is important
in physiological, pathophysiological, and clinical
studies. Although the sphincter of Oddi (SO) can be
evaluated with manometry, this technique has several
limitations. This may explain the difficulties in identifying pathophysiological mechanisms for dysfunction
of the SO and in identifying patients who may
benefit from certain therapies. To encompass problems
with manometry, methods such as the functional lumen
imaging probe (FLIP) technique have been
developed to study GI sphincters. This study set about
miniaturising the FLIP probe and validating it for
measurements in the SO. In order to get a better
physiological understanding of the SO the aims were
to show the sphincter profile in vivo and motility
patterns of SO in pilot studies using volunteers that
were experiencing biliary type pain but had normal SO
manometry. Methods The SO probe was constructed
to measure eight cross-sectional areas (CSA) along a
length of 25 mm inside a saline-filled bag. To validate
the technique for profiling the SO, six perspex
cylinders with different CSAs were measured nine
times to assess reproducibility and accuracy.
Key Results Reproducibility and accuracy for these
measurements were good. The probe performed well in
bench tests and was therefore tested in four humans.
The data indicated that it was possible to make
distensions in the human SO and that a geometric
sphincter profile could be obtained. Conclusions &
Inferences The probe will in future studies be tested
for diagnostic purposes related to sphincter of Oddi
diseases.
full article »»»

Development and clinical application of new scintigraphic and manometric methods for the diagnosis of functional disorders of the gallbladder and the sphincter of Oddi
Authors: Madácsy L.
To summarize our results, an optimal diagnostic and therapeutic approach may be suggested in patients with functional biliary disorders. It is worth mentioning that the diagnostic strategy should be modified individually in accord with the clinical status of the patient. Consequently, the clinical value and diagnostic role of QHBS must be evaluated in relation to the degree of biliary obstruction. ERCP must be performed in all cases when the
obstruction is a high-grade one, when gallstone disease is suspected by the ultrasound, or when AN-augmented QHBS suggests an organic biliary obstruction. If no clinical sign of biliary obstruction is evident in a patient with functional biliary pain, it is reasonable to start
with AN-augmented QHBS to determine bile flow abnormalities. After the exclusion of organic causes, the probability of SO dyskinesia or GB dyskinesia is high if a typical clinical picture is accompanied by a suggestive QHBS result. The clinician should then decide
whether ESOM is indicated to establish the diagnosis. The latter also depends on the therapeutic plan, since the QHBS results might not be sufficient to plan an operative
endoscopic procedure such as EST, which is not without risk. In contrast, if drug therapy is planned, positive scintigraphy should be sufficient for the initiation of medical treatment. It is generally accepted and proved by long-term follow-up studies that in patients with SO
stenosis (SOD of biliary group I) EST is the treatment of choice [98-100]. As these patients with SOD of biliary type I invariably benefit from EST, ESOM is not necessary [100]. In contrast, in patients with SO dyskinesia (biliary groups II and III) ESOM is needed to perform in order to prove the elevated SO BP as an indication of EST, since in patients with SO dyskinesia and a normal SO BP EST did not prove to be more beneficial than the sham procedure [101]. Moreover, in another follow-up study, a sustained symptomatic
improvement was detected after EST in only 8% of the patients with SOD of biliary type III (functional group) [102]. Therefore, with regard to the high incidence of complications following EST in patients with non-dilated ducts, it should be considered only after a failure
of conservative therapy in the subgroup of patients with an elevated SO BP [103]. If all these tests are negative, then a provocation test may be considered, such as a prostigmine-morphine test combined with QHBS. Provocation tests might unmask subtle abnormalities, such as hyperreactivity of the SO, which explain the patient`s complaints. In patients with ABP, and an intact GB with normal SO motility, QHBS combined with CCK and GTN coadministration should be performed to establish the diagnosis of GB dyskinesia.
To summarize the present work, we proved that QHBS is a useful method in the diagnosis of functional disorders of the biliary tract. We established a close correlation
between the bile flow determined by QHBS and the SO pressure measured by ESOM. We applied AN and prostigmine-morphine augmentations, QHBS thereby becoming a real
functional test in the diagnosis of SOD. We combined QHBS with CCK and GTN coadministration in patients with intact GB and ABP, which could be a reliable method in the
diagnosis of GB dyskinesia. We hope that, in the future, these methods will gain general acceptance as a first line diagnostic test in patients with suspected biliary dyskinesia.
full article »»»

Comparison of the dynamics of bile emptying by quantitative hepatobiliary scintigraphy before and after cholecystectomy in patients with uncomplicated gallstone disease.
Authors: Madácsy L, Toftdahl DB, Middelfart HV, Hojgaard L, Funch-Jensen P.
PURPOSE: Quantitative hepatobiliary scintigraphy, a noninvasive method frequently used to diagnose several biliary tract disorders, shows abnormalities in bile secretion and outflow. It is well known that there are wide variations in the normal pattern of bile emptying, but the effect of cholecystectomy on the bile flow has not yet been investigated. The goal of the current study was to examine the dynamics and normal variations of bile flow by quantitative hepatobiliary scintigraphy before and after cholecystectomy in a group of patients with uncomplicated gallstone disease. METHODS: Twenty patients were evaluated before and after cholecystectomy through cholecystokinin octapeptide-augmented quantitative hepatobiliary scintigraphy, and quantitative parameters of bile emptying (Tmax: time to peak activity, T1/2: half-emptying time before and after cholecystokinin octapeptide and duodenum appearance time) were determined and then compared. RESULTS: Before operation, the bile outflow displayed wide variations, with a moderately delayed common bile duct emptying time in some patients. After cholecystectomy, the T1/2 of the common bile duct decreased significantly when compared with the preoperative status, with only minor patient-to-patient variation, indicating uniformly faster bile emptying (common bile duct T1/2 before and after operation: 30.5 +/- 14.8 and 18.8 +/- 2.6 min, respectively). Cholecystokinin octapeptide administration caused rapid bile outflow from the common bile duct, with a significant decrease in the T1/2 parameters before and after cholecystectomy. CONCLUSIONS: In patients with their gallbladders in situ, the bile emptying rate showed wide variations and may be moderately slow without distal common bile duct obstruction. After cholecystectomy, the rate of bile emptying accelerated and showed only minor variations, thereby increasing the sensitivity of quantitative hepatobiliary scintigraphy for showing partial biliary obstruction.
full article »»»